Allogene’s CAR T-cell Therapy Triggers Durable Anti-Tumor Response in Animal Model
ALLO-715, Allogene Therapeutics‘ donor-derived CAR T-cell therapy, can trigger a durable anti-tumor response in mice with multiple myeloma, and maintain its characteristics and anti-tumor activity after large-scale manufacturing, a study says.
The preclinical findings were reported in the study, “Preclinical Evaluation of Allogeneic CAR T Cells Targeting BCMA for the Treatment of Multiple Myeloma,” published in Molecular Therapy, and had been previously presented at the 60th American Society of Hematology (ASH) Annual Meeting & Exposition.
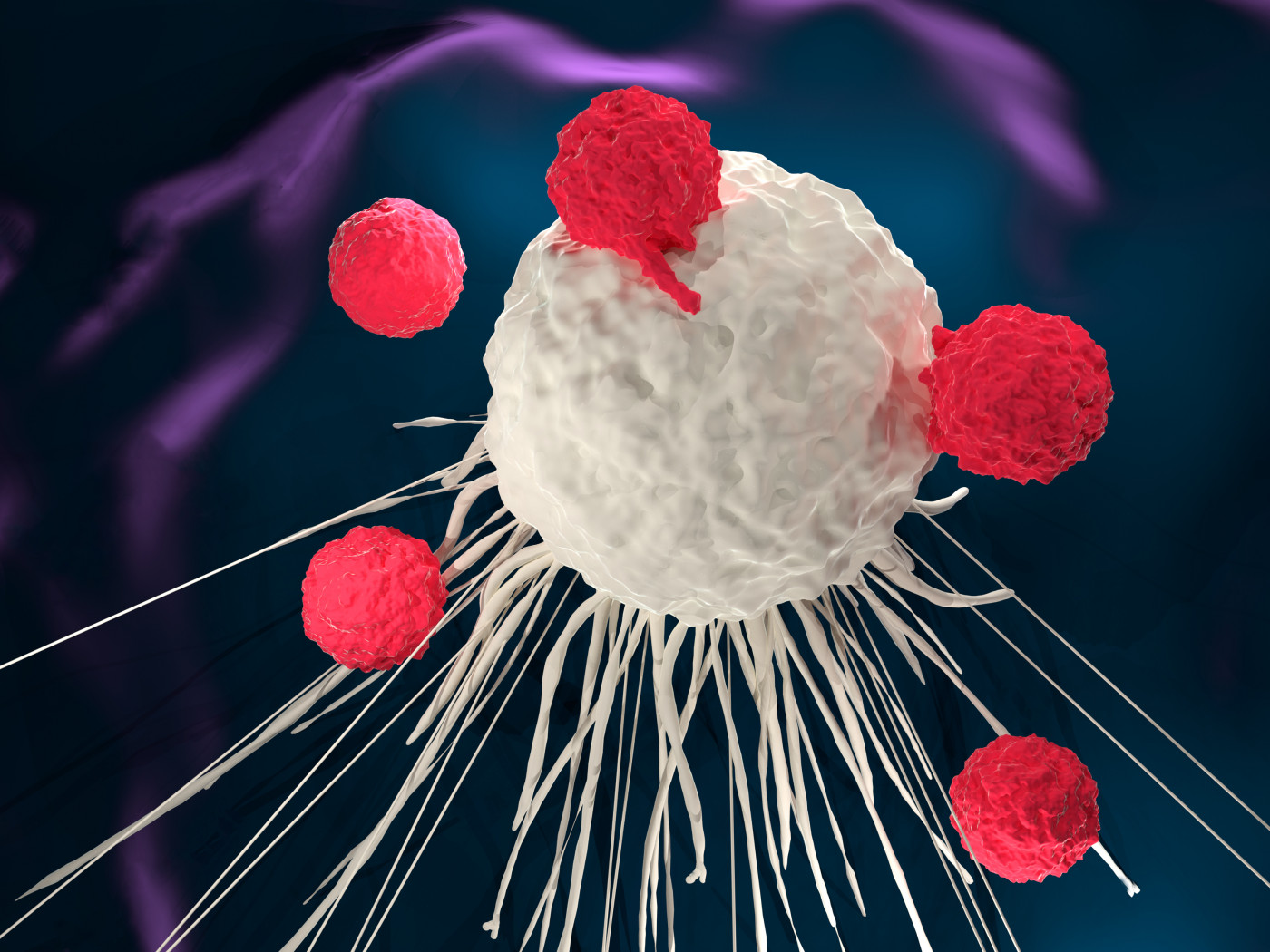
Chimeric antigen receptor T-cell therapy, more commonly known as CAR-T cell therapy, is a type of immunotherapy in which researchers collect a patient’s T-cells — immune cells with anti-cancer activity — and re-engineer them in the lab so that they can recognize and eliminate cancer cells. The treated cells are then inserted back into the patient’s body to fight the tumor.
Allogene’s ALLO-715 are genetically-modified human T-cells that specifically recognize and eliminate malignant cancer cells containing the B Cell Mature Antigen (BCMA), while leaving healthy cells unharmed. But instead of being collected from patients, researchers harvest T-cells from healthy donors, allowing the therapy to be offered off-the-shelf.
Investigators now are testing ALLO-715 as a treatment for multiple myeloma and other types of BCMA-positive blood cancers in animal models of disease.
To minimize the risk of graft-versus-host disease (GvHD), a serious complication in which the transplanted T-cells from the healthy donors start attacking the host’s body, researchers used gene-editing tools to modify the donor T-cells so they would only recognize and attack cancer cells containing BCMA.
Then, investigators added another safety layer by including a CD20-based off-switch allowing them to destroy genetically-modified T-cells in the presence of Rituxan (rituximab), if needed.
Results showed that ALLO-715 triggered a strong and durable anti-tumor response in animals with multiple myeloma treated with human cytokines, which are molecules that mediate and regulate immune and inflammatory response.
Further analysis demonstrated these genetically-modified T-cells were able to maintain their characteristics and anti-tumor activity after being expanded at a large scale, suggesting this new donor-derived CAR T-cell therapy may be a promising treatment candidate for patients with multiple myeloma.
“These preclinical findings validate advancing ALLO-715 produced via our proprietary manufacturing process to target BCMA, which is expressed in multiple myeloma,” David Chang, MD, PhD, the president, CEO, and co-founder of Allogene, said in a press release.
Allogene Therapeutics is now planning to file an Investigational New Drug Application with the U.S. Food and Drug Administration, and launch the first human Phase 1 clinical trial for ALLO-715 later this year. The trial will include multiple myeloma patients who failed prior therapies.
ALLO-715 is based on Celectis‘ TALEN gene-editing technology. The preclinical study was done in collaboration with Celectis and Pfizer‘s Cancer Immunology Discovery unit.






