Finding That Immune Cells Interact Could Lead to Myeloma Therapies, Study Suggests
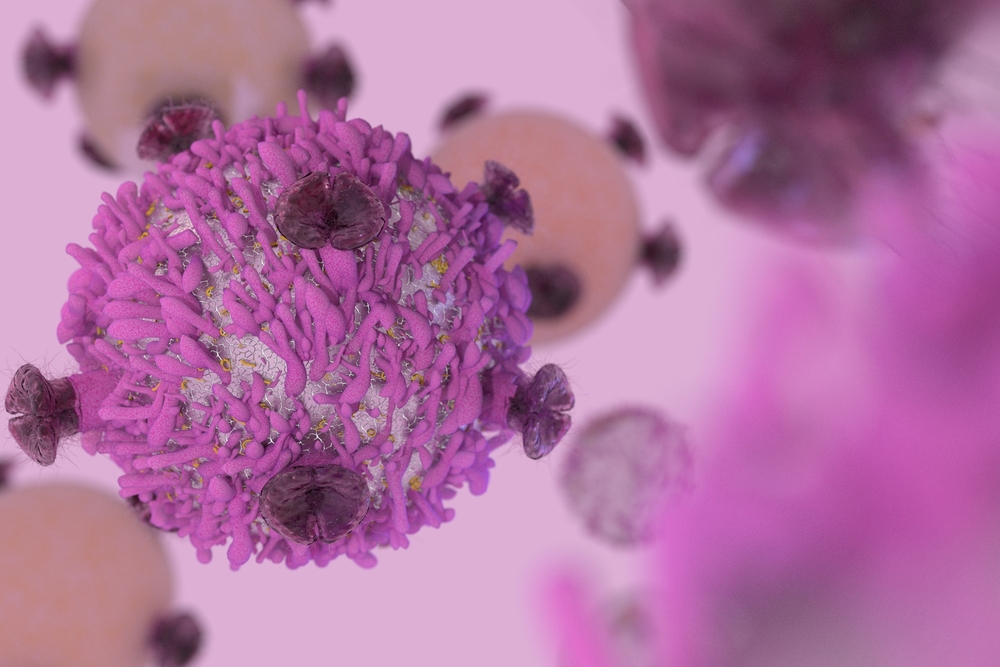
One kind of immune cell helps another stay active for years against invaders, a finding that could lead to therapies for autoimmune diseases and certain kinds of cancer, according to a study.
The discovery that T-cells regulate plasma cells could provide insight into how some plasma cells become faulty, contributing to the development of such diseases, researchers said.
The study, “T Regulatory Cells Support Plasma Cell Populations in the Bone Marrow,” was published in Cell Reports.
Christopher A. Hunter, the study’s lead author, has been investigating how the immune system responds to infection with the parasite Toxoplasma gondii.
Hunter, colleagues at the University of Pennsylvania School of Veterinary Medicine (Penn Vet), and international research collaborators used high-tech microscopes to examine the behavior of immune cells and other structures in living organisms.
They discovered that mice exposed to T. gondii lost the plasma cells in their bone marrow. When the team controlled the infection, however, the plasma cells returned.
“We don’t know whether these cells leave the bone marrow or die there during infection, but, either way, they are gone,” Glatman Zaretzky, one of two trainees in Hunter’s lab who conducted the study, said in a press release. “And that set up a great system to understand what kinds of cellular interactions normally create the hospitable environment and allow the plasma cells to remain there.”
The researchers found regulatory T-cells, or Tregs, in the same locations as plasma cells — near blood vessels. As happened with plasma cells, when mice were infected with T. gondii, the number of Tregs in the bone marrow dropped dramatically.
A mouse model helped the team learn whether the two cell types interact. The researchers tagged the mouse model’s plasma cells with yellow fluorescent markers and its Tregs with green ones. They discovered that the Tregs and plasma cells interact in bone marrow for a long time.
“No one had put these two cell types together before,” said Hunter, the Mindy Halikman Heyer Distinguished Professor of Pathobiology and chair of the Department of Pathobiology at Penn Vet. “Yet, when we looked, we saw that these interactions were not rare but were frequent and sustained.”
Researchers also found that Tregs were needed to maintain plasma cells. When Treg survival was enhanced during infection, the number of plasma cells in the mouse model increased. When the team reduced the Treg-cell count, the number of plasma cells fell.
The findings offer cues about why plasma cells can stay in the body a long time. The cells remain long after rushing to the site of a vaccine or destroying an infection, to continue working against invaders.
An important conclusion of the research was that interfering with the interaction between T-cells and plasma cells could lead to treatments for diseases caused by plasma cells, such as autoimmune diseases and multiple myeloma.
“If we can understand what controls these long-lived plasma cells, then maybe we can augment that interaction, making more plasma cells to, for example, enhance vaccine efficiency,” Hunter said. “Or, if you want to limit autoimmunity or cancer, maybe there is an opportunity to disrupt this niche to mitigate some of those conditions.”