Dendritic Cell Immunotherapy Failed to Gain Upper Hand in Relapsed, Refractory Myeloma in Study
A new type of dendritic cell-based immunotherapy triggered an immune response in the majority of patients in a small Phase 1 trial (NCT02248402) of relapsed or treatment-resistant multiple myeloma. But that was not enough to combat the cancer, as the best clinical response was a temporary stabilization of disease.
Researchers are now focusing on increasing the effectiveness of the treatment, named VAX-DC/MM. The study, “A phase 1 clinical study of autologous dendritic cell therapy in patients with relapsed or refractory multiple myeloma,” was published in the journal Oncotarget.
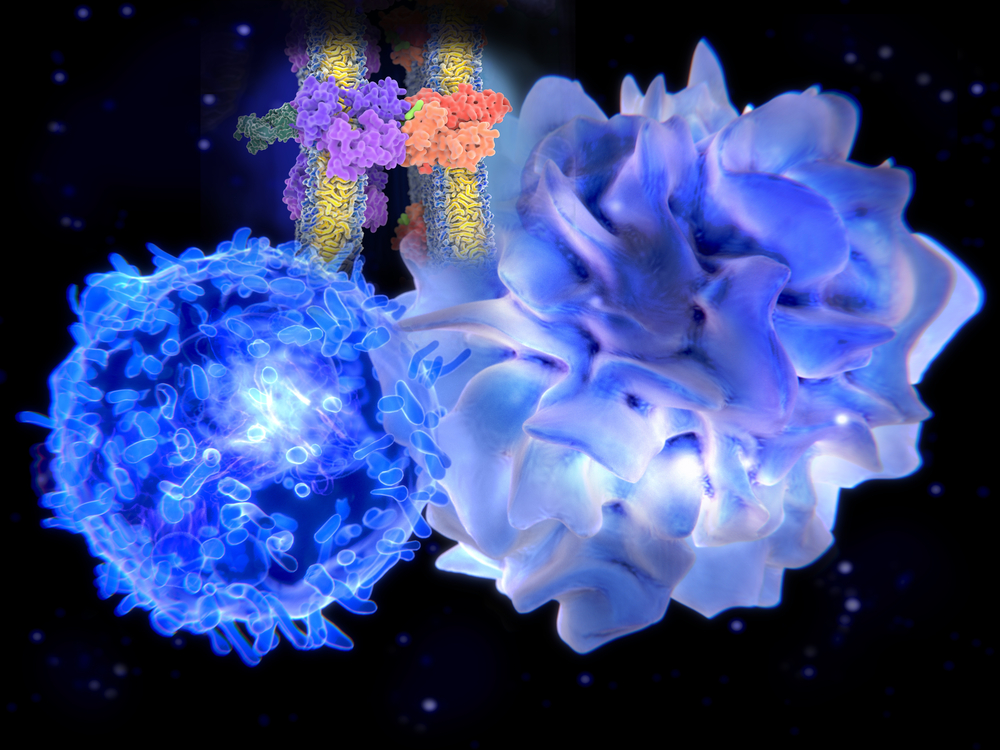
VAX-DC/MM is an approach that harnesses the body’s system to alert immune cells to the presence of a threat. It uses dendritic cells, which ingest intruders, and displays pieces of them on their surface to attract attention to an infection or tumor.
Researchers at the Chonnam National University Hwasun Hospital in South Korea developed a treatment in which they use the patient’s own dendritic cells, which are fed myeloma cells irradiated with ultraviolet B. Once these cells are injected back into a patient, they activate T-cells, which in turn launch an immune attack.
The trial recruited 12 patients, all of whom had received previous treatment. The median number of previous treatment courses was five, and 75 percent of the patients had undergone an autologous stem cell transplant.
Three patients received a lower dose of 5 million cells, while nine received 10 million. The cells were injected into the skin once a week for four weeks. Researchers analyzed immune system and clinical responses only in the nine patients who received a higher dose.
Assays showed that 77.8% had an immune response following the treatment. The proportion of patients who also had a clinical response was 66.3%, with one patient having a minor response and five stabilizing. The remaining 33.3% of the patients showed disease progression despite treatment.
The patients were followed for a median of 16.1 months, during which eight of the nine patients progressed. The median progression-free survival was 2.9 months.
The most common adverse effects of the treatment were local reactions at the injection site. Other side effects included muscle pain and fever, as well as low numbers of white blood cells and platelets.






