Myeloma Therapies Advancing Rapidly, Says Expert at Sloan Kettering
In a video posted on Healio’s Hematology-Oncology page, Dr. Ola Landgren, chief of the myeloma service at Memorial Sloan Kettering Cancer Center in New York City, speaks about new treatments and ongoing discoveries in the field of multiple myeloma.
A lot is taking place, quickly, according to Landgren. “I think that the myeloma field is changing almost every six months with the current pace and with access to all these new technologies,” he said.
He particularly spoke of three drugs, approved by the U.S. Food and Drug Administration in November 2015. The trio — two antibodies called Darzalex (daratumumab) and Empliciti (elotuzumab) and one proteasome inhibitor called Ninlaro (ixazomib) — were approved for relapsed or refractory myeloma, in patients who have tried one or several rounds of conventional treatment.
These drugs make use of entirely new mechanisms to kill the cancer, and, according to Landgren, results from the clinic suggest that a very high proportion of patients get a good response when treated with these drugs. Now, trials are exploring if the drugs might also be of use in earlier settings and in newly diagnosed patients. Other studies are investigating if these newcomers can be combined with older, available drugs to boost their efficiency.
Landgren also believes that the new multiple myeloma medications will be bundled together in combinations with available drugs in the future, where a four-drug combo can be used in newly diagnosed patients. He foresees that such combinations could produce complete responses in up to 80 percent or 90 percent of patients.
He thinks that new data from clinical trials will put pressure on the current standard paradigm of chemotherapy with the drug Alkeran (melphalan) and stem cell transplants. Today, there is not enough evidence supporting that patients using the new drugs have equally good survival as patients on the standard treatment, but preliminary data suggests that if patients reach a sufficiently good response on the new drugs in combination, their survival is as good as with chemotherapy and stem cell transplants.
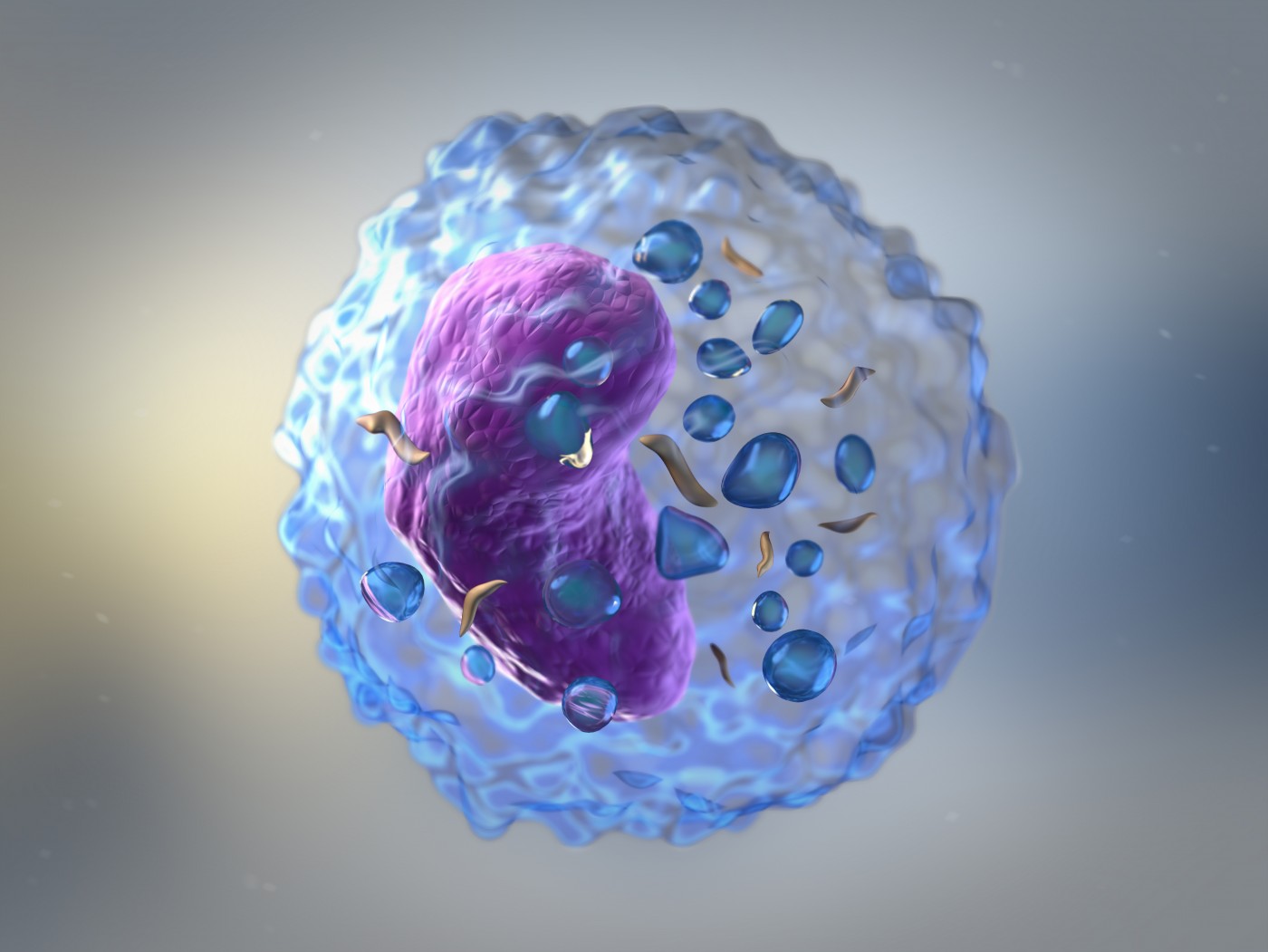
Treatment development is not limited to antibodies, and Landgren particularly mentioned CAR T-cell therapy — a method where a patient’s own immune T-cells are taken from the body and genetically modified before they are released back, launching attacks on tumors.
He pointed out that there is very little data supporting CAR T-cell therapy in multiple myeloma. Late last year, the National Cancer Institute in Bethesda presented positive results from a trial involving a small number of patients, who responded with dramatic improvements to the treatment.
The Kettering Cancer Center is working to start a CAR T-cell program, which Landgren thinks will be up and running in nine to 12 months, but also other U.S., European, and Asian institutions are developing CAR T-cell strategies for multiple myeloma. We will find out in due time if such approaches might replace or complement new treatment strategies, Landgren said.
“I think that until we have a cure for multiple myeloma, every effort that moves the field forward or advances the opportunities for patients that are relapsing, are strongly needed,” he said, adding that he has an optimistic view of developments in the myeloma field. “The future looks very bright, but there is more work to be done.”