Weighing Myeloma Cells Could Predict Treatment Responses, MIT Study Shows
Weighing individual cancer cells could help doctors predict how multiple myeloma patients will respond to treatments, a Massachusetts Institute of Technology study reports.
The findings could help doctors choose the right drug for the right patient, the team argued in the article they published in the journal Nature Communications. The title of the piece is “Determining therapeutic susceptibility in multiple myeloma by single-cell mass accumulation.”
In “infectious diseases, antibiotic susceptibility testing based on cell proliferation has been extremely effective for many decades,” Scott Manalis, an MIT professor who was the senior author of the study, said in a press release.
Such tests have not been available in cancer, however, so doctors don’t know which myeloma drug might benefit which patient.
Developing tumor cell tests has been “challenging, in part because the cells don’t always proliferate upon removal from the patient” for testing, said Manalis, a biological and mechanical engineering professor who also works at the university’s Koch Institute for Integrative Cancer Research. “The measurement we developed doesn’t require proliferation.”
The method, weighing individual cancer cells, is 10 to 100 times more accurate than other techniques for assessing patients outcomes. The team has refined the method for decades. But it recently decided to see whether it can be used to predict patients’ responses to drugs.
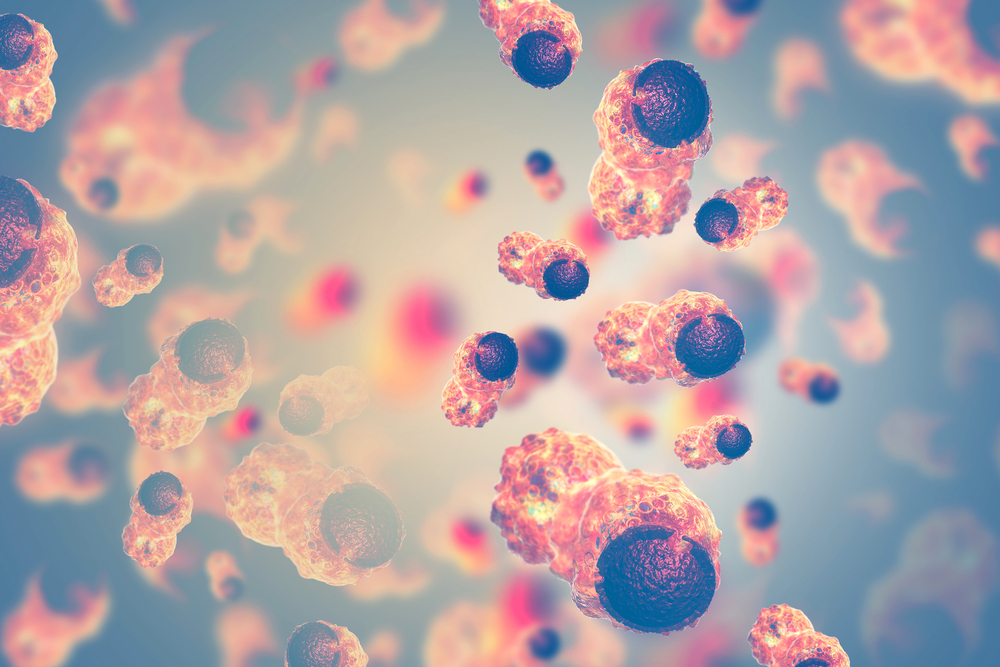
Last year, the team discovered that the rate at which a cell gains weight can show how sensitive it is to treatment. If cells are responding to a treatment, then the rate slows, they said. Cells that are resistant to treatment continue to grow at the same rate.
For the new study, the team used these insights to test three cancer drugs, alone or in combination, on cells from nine myeloma patients. They compared the cells’ weight gains with how patients fared from treatment.
Changes in cell weight, it turned out, mirrored responses to treatment. The response measure the team used was levels of blood markers for myeloma.
“When the clinical biomarkers showed that the patients should be sensitive to a drug, we also saw sensitivity by our [cell weight] measurement,” said Mark Stevens, a scientist at the Dana-Farber Cancer Institute who was the study’s lead author. “In cases where the patients were resistant, we saw that in the clinical biomarkers as well as our measurement.”
Many myeloma patients respond to treatment initially, then relapse. The MIT team believes their cell-weight method could help predict a relapsed patient’s response to the next treatment.
“At this time of relapse, we would take a bone marrow biopsy from a patient, and we would test each therapy individually or in combinations that are typically used in the clinic,” Stevens said. “At that point, we’d be able to inform the clinician as to which therapy or combinations of therapies this patient seems to be most sensitive or most resistant to.”
The team is laying groundwork for a clinical trial to validate their cell-weight approach, while also looking at whether it is equally sensitive in other cancer types.