Microfluidic Device May Replace Bone Marrow Biopsies for Myeloma
Patients with multiple myeloma soon may be diagnosed and followed solely with the use of a blood sample, avoiding the painful process of collecting a bone marrow biopsy.
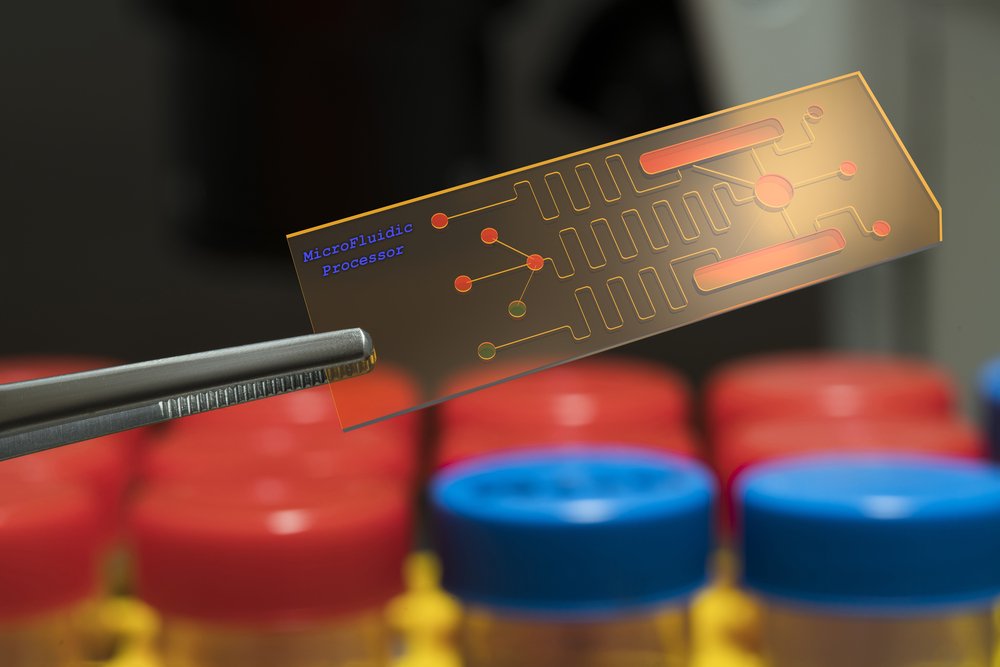
Researchers at the Massachusetts Institute of Technology (MIT) have developed a microfluidic device that grabs plasma cells — the myeloma cancer cells — from blood samples, suggesting it could be used as a diagnostic and prognostic test during treatment.
The study, “Isolation of Circulating Plasma Cells in Multiple Myeloma Using CD138 Antibody-Based Capture in a Microfluidic Device,” was published in Scientific Reports.
“Procedures of the traditional tissue biopsy are painful, associated with complications such as potential infections, and often available only in central hospitals which require patients to travel long distances,” study first author Mohammad Qasaimeh, PhD, said in a press release. “Capturing plasma cells from blood samples can serve as a liquid biopsy, which can be performed in clinics as often as required, and serve as a diagnostic and prognostic test during and after chemotherapy treatment. Moreover, captured cells can be used for drug testing and thus serve as a tool for personalized medicine,” he said.
The newly developed technique builds on a microfluidic design previously developed by George Whitesides, PhD, a professor of chemistry at Harvard University.
Whitesides and colleagues created a small microchip, in which the fluid channel is made of repeated V-shaped grooves, making the fluid swirl about in eddies, rather than passing the microchip straight through. This design increases the chances of cells within the fluid making contact with the bottom of the device.
The researchers reproduced this microfluidic design, but coated the microchip’s bottom with an antibody that targets the CD138 molecule, present in the membrane of circulating plasma cells. The microchip was about the size of a glass slide.
When the team passed small, one-milliliter blood samples through the device, the antibodies in the microchip worked as tiny velcro pads, grabbing any passing plasma cells while letting other blood cells flow out of the device. Then, researchers could count how many plasma cells were in that blood sample. In addition, they also could determine the types of antibodies each cell secreted.
Plasma cells are the white blood cells that produce antibodies to fight off infections, but when they become malignant in myeloma patients they produce large amounts of abnormal antibodies, which often cause the disease’s symptoms.
Plasma cells can produce two kinds of antibodies, known as kappa- and lambda-type. The ratio of these antibodies is usually a good indicator of disease progression.
The researchers tested their device with blood samples from healthy subjects and myeloma patients. They found that while healthy subjects had a low number of circulating plasma cells (two to five per milliliter of blood), those with myeloma had substantially more cells in circulation (45 to 184 per milliliter).
They also found that the ratio of lambda and kappa-type antibodies matched with the patient’s condition, which further validated the device’s accuracy.
But, to their surprise, the team found that while patients in remission had normal levels of the antibodies, they still had higher number of plasma cells in the blood than healthy subjects. Researchers believe the device may provide more subtle information about a patient’s state, which ultimately could improve his management.
“When patients go into remission, their antibody levels can look normal,” said Rohit Karnik, PhD, an associate professor in MIT’s Department of Mechanical Engineering. “But we detect a level of circulating plasma cells that is above the baseline. It’s hard to tell whether these cells are cancerous, but at least this technique is giving us more information. With the ease of a blood draw, this may enable us to track cancer in a much better way,” he said.
Karnit added that in the future the device may allow the collection of plasma cells to perform genetic and mutational tests, which should help doctors further characterize a patient’s disease.
“We can capture and stain these cells in the device, which opens the possibility of studying whether there are new mutations in the cells,” Karnik said. “With cancers like multiple myeloma, even for patients in remission, cancer can recur. Detecting the level or mutation of plasma cells in blood might provide an early detection method for these patients.”