Multiple Myeloma Cancer Stem Cells Decreased with Novel Antibody Medi-551
A preliminary clinical study at Johns Hopkins Kimmel Cancer Center demonstrated that antibody treatment could decrease by half the number of cancer stem cells, which control the progression of cancer in almost all patients suffering from multiple myeloma.
The efficiency of the antibody MEDI-551 was studied in 15 patients suffering from multiple myeloma who had already undergone regular chemotherapy by lenalidomide and dexamethasone. The researchers published their observations at the American Association for Cancer Research (AACR) Annual Meeting 2016 in New Orleans.
Lead scientists William Matsui and Carol Ann Huff investigated the influence of the antibody on the number of cancer stem cells in bone marrow and blood for seven months.
According to their findings, the number of cancer stem cells in bone marrow was increased by approximately 2.5-fold after two monthly treatments of lenalidomide and dexamethasone, while applying MEDI-551 twice in the next two months reduced the count of cancer stem cells by half in 14 of the 15 patients.
For five multiple myeloma patients who did not undergo antibody treatment, the number of cancer stem cells was raised by 9.3-fold after an average of four months of therapy with lenalidomide and dexamethasone. No serious side effects were registered among the patients treated by the antibody.
Matsui and Huff belong to the research team that first isolated cancer stem cells in multiple myeloma. Their ongoing research demonstrated how cancer stem cells contribute to relapse multiple myeloma, in addition to finding new routes to target stem cells supporting drug discovery and development.
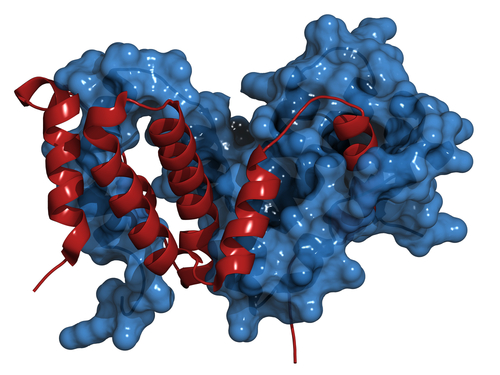
MEDI-551 targets a protein called CD19 found on the surface of multiple myeloma cancer stem cells, Matsui said. “We chose to carry out this clinical trial in newly diagnosed patients because our original data showed that CD19 was almost always expressed by myeloma stem cells in these patients, whereas we don’t know if that is the case in more advanced patients,” he said.
The scientists studied two different methods to count the cancer stem cells: in bone marrow and in blood. “We wanted to see if these two assays gave similar results, and in this clinical trial, they were almost identical,” Huff said. “Since it is much easier to draw blood than bone marrow from our patients, we think that we can primarily use blood to track multiple myeloma stem cells in the future.”
In most of the patients, the number of cancer stem cells decreased after three doses of MEDI-551; however, in two of the patients whose cancer had had grown or spread, the cancer stem cell number grew.
Matsui, Huff, and their co-workers plan to carry out additional studies to determine the long-term effects of MEDI-551 and to show how the antibody can be applied in combination with other therapies.
“In other studies at Johns Hopkins, we have found that antibody therapies can work much better after a bone marrow transplant, especially allogeneic transplants, where patients receive bone marrow cells donated from a relative,” Matsui said.






