CRISPR-edited T-cells Safely, Effectively Target Cancer Cells in Myeloma Patients, Early Phase 1 Data Suggests
A new approach using genetically modified T-cells — via CRISPR-Cas9 gene editing technology — safely and effectively targets cancer cells in patients with advanced multiple myeloma, preliminary data from a U.S.-based Phase 1 study show.
Despite their preliminary nature, researchers believe these findings raise hope that this approach may be used in multiple areas of gene therapy research.
The results will be presented in “First-in-Human Assessment of Feasibility and Safety of Multiplexed Genetic Engineering of Autologous T Cells Expressing NY-ESO -1 TCR and CRISPR/Cas9 Gene Edited to Eliminate Endogenous TCR and PD-1 (NYCE T cells) in Advanced Multiple Myeloma (MM) and Sarcoma,” an oral presentation at the 61st ASH Annual Meeting & Exposition, to be held Dec. 7-10, in Orlando. The expo is hosted by the American Society of Hematology.
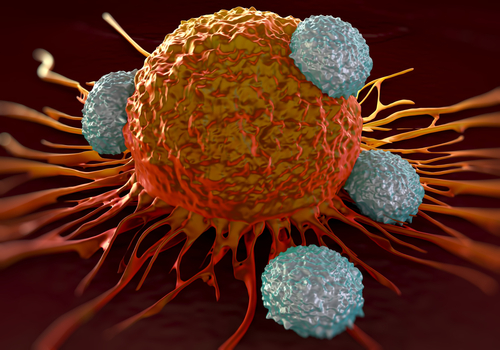
T-cells, a type of white blood cell, recognize foreign molecules through specific membrane receptors called TCRs. TCRs can be genetically altered to specifically recognize and kill tumor cells, a strategy called TCR-engineered T-cell therapy.
Much like CAR T-cell therapy, the approach requires the isolation of T-cells from a patient’s blood draw. The cells are genetically modified and infused back into the patient. But instead of including a receptor against a cancer protein, like BCMA, this technique removes genes that may hinder the cells’ ability to target cancer cells. It also arms cells with a modified TCR against a cancer target, making sure they are only active when they encounter their target.
A previous Phase 1/2 clinical trial (NCT01352286) evaluated the therapeutic benefits of using T-cells genetically modified to produce a TCR that specifically recognizes NY-ESO-1 — a protein highly present in various tumors, including approximately 30% of multiple myeloma cases. The trial used the therapy to treat 25 high-risk or relapsed myeloma patients.
The results showed that the treatment was generally safe and kept patients alive and progression-free for a median of 13.5 months. These individuals went on to live for a median of 35.1 months after enrolling in the trial.
The pilot Phase 1 study (NCT03399448) is currently evaluating the five-year safety and effectiveness of using a new engineered T-cell, called NYCE T-cell, to treat up to 18 patients with advanced myeloma, sarcoma, or melanoma.
This new T-cell therapy combines the introduction of the NY-ESO-1-directed TCR — through a harmless virus that delivers a gene carrying that genetic information — and the use of CRISPR/Cas9 technology. It is designed to delete two genes with instructions to produce the natural TCR, and a third gene with instructions to produce the PD-1 receptor.
Activation of the PD-1 receptor in T-cells by its ligand, PD-L1, is part of a well-known and powerful mechanism of immune evasion by cancer cells. These cells increase PD-L1 levels on their cell surface, so that they bind to and activate PD-1 on T-cells, suppressing their immune responses.
The removal of these two receptors is thought to boost T-cell anti-tumor activity and increase their persistence in the body. It works by reducing the competition between the natural TCR and the NY-ESO-1-directed TCR, decreasing T-cell exhaustion, and maintaining T-cell activity in the presence of PD-L1 in tumor cells.
The study, led by the University of Pennsylvania in collaboration with the Parker Institute for Cancer Immunotherapy (PICI) and Tmunity Therapeutics, is the first-ever U.S. clinical trial testing a CRISPR-edited cell therapy.
“We leaned heavily on our experience as pioneers of the earliest trials for modified T-cell therapies and gene therapies, as well as the strength of Penn’s research infrastructure, to make this study a reality,” Carl June, MD, the study’s senior author and the director of the Center for Cellular Immunotherapies in the Abramson Cancer Center of the University of Pennsylvania, said in a press release.
Study participants are being recruited from the Abramson Cancer Center. To be eligible, patients must have NY-ESO-1-producing tumors and be able to produce HLA-A*02, a cell-surface protein involved in immune system regulation. More information on recruitment contacts can be found here.
Data from the study’s first three participants — two with multiple myeloma and one with sarcoma, another type of rare cancer — all treated with NYCE T-cells, will be presented at the meeting.
The myeloma patients were two women, ages 62 and 67, who had received between seven and eight previous lines of therapy, including two immunomodulatory treatments, two proteasome inhibitors, the monoclonal antibody Darzalex (daratumumab), and two to three autologous stem cell transplants (ASCTs).
The participants received other therapies as needed while they waited for their T-cells to be manufactured, as well as a short course of chemotherapy to eliminate natural immune cells before receiving the NYCE T-cells.
Analysis on blood and tumor samples from the first two participants — the older myeloma patient and the sarcoma patient — showed that a single administration of the NYCE T-cells directly into the patients’ bloodstream resulted in the expansion and survival of these cells, which were found to bind to their tumor target.
After two months, the older woman showed signs of disease progression, while cancer remained stable in the sarcoma patient three months after treatment. The researchers noted that it was too early to perform similar analyses in the younger woman with myeloma, the last participant to enter the study.
To date, the therapy was well-tolerated in all patients, with no treatment-related serious adverse events.
“This trial is primarily concerned with three questions: can we edit T-cells in this specific way? Are the resulting T-cells functional? And are these cells safe to infuse into a patient? This early data suggests that the answer to all three questions may be yes,” said Edward A. Stadtmauer, MD, the study’s principal investigator and the one presenting the findings at the meeting.
Researchers will continue to follow the participants. Long-term data will help to determine the true potential of this new approach, the investigators said. Nevertheless, they are optimistic about the early results, and believe this approach may be used to treat several diseases.
“These early findings are the first step as we determine if this new, breakthrough technology can help rewrite how we treat patients with cancer and perhaps other deadly diseases,” said Sean Parker, founder and chairman of the Parker Institute.
“CRISPR editing could be the next generation of T cell therapy, and we are proud to be a part of the first human trial in the United States,” Parker added.






